Blog

Why We Test Insulin Blood Levels
Customers who order our blood test panels often ask why we measure fasting insulin.
One reason is that higher fasting insulin levels are correlated with lower life expectancy’ and increased risks of cancer2-5 and cardiovascular disorders.6-8
Insulin production is regulated by blood sugar levels and hormones. Fasting insulin increases in response to insulin resistance.9,10
At first, higher insulin levels can initially help drive glucose out of the blood into cells.10
As insulin resistance worsens, even greater insulin secretion fails to adequately normalize blood glucose.10
A missed opportunity for early diagnosis occurs when fasting insulin is omitted from blood panels that measure glucose and Al c.
Higher levels of insulin can temporarily reduce glucose and Al c in a way that masks glycemic control issues.10
In other words, glucose and A1c may appear “normal” on blood test results. But without testing fasting insulin, this may create a false sense of security by not recognizing that the “excess” insulin is helping to keep glucose and Alc within ) acceptable ranges.11
Before full-blown type II diabetes manifests, subop¬timal glycemic control is associated with increasing risks of the most common diseases12 of aging.13-16
Further, worsening glycemic control can silently contribute to diabetes, leading to peripheral nerve damage (neuropathy), chronic kidney disease, and/ or loss of vision (retinopathy).17
Newly diagnosed diabetics often ask why so many morbidities afflict them so quickly. The answer is these pathologies were festering for years as a result of suboptimal metabolic control, which could have been identified earlier with proper blood tests.
Some studies have shown that fasting insulin levels are a more accurate predictor of cardiometabolic risk, compared to tests for insulin resistance.18,19
One of the most serious global health problems today is metabolic disorders related to obesity and insulin resistance.20-2 Effective methods (diet and exercise) can slow or halt progression to type II diabetes—but prevention is critical.
That’s why it’s essential to include fasting insulin with glucose and Alc blood testing to get a more accurate understanding of your glycemic status.
Type II diabetes is surging higher worldwide among all age groups.
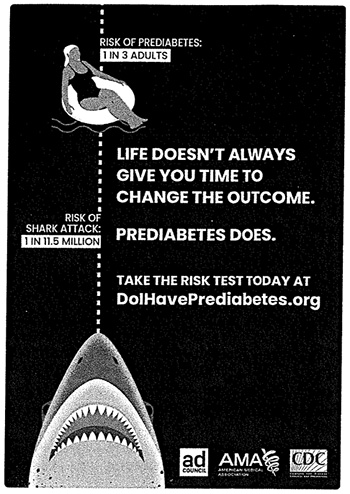
The Centers for Disease Control and Prevention is running public service ads (one copied on this page) warning that one in three American adults is at risk for prediabetes.20
The term “prediabetes” can be misleading.
Few realize that the initial stages of glucose imbalance inflict severe tissue damage. This happens before full-blown type II diabetes is officially diagnosed.6
These pathologies are not limited to adults. There was an astounding 95% increase in Americans under age 20 living with type II diabetes between 2001-2017.22
Need for Early Intervention
 Most cases of type II diabetes begin when cells slowly become resistant to insulin.20
Most cases of type II diabetes begin when cells slowly become resistant to insulin.20
When this occurs, glucose buildup in blood causes the pancreas to secrete higher levels of insulin to force glucose into cells. This temporarily helps compensate for insulin resistance in target tissues (e.g., skeletal, muscle, liver).
During the period of insulin resistance, weight gain may be an outward sign of loss of glycemic control. This happens as elevated levels of glucose + insulin contribute to unwanted fat storage.1,23
Weight gain and physical inactivity increase the risk of developing insulin resistance.2
As insulin resistance worsens, insulin levels often rise as the pancreas attempts to compensate and literally force glucose into target tissues that have become resistant to the action of insulin at a cellular level.1
 If a blood test reveals high fasting insulin before glucose and Alc become elevated, this provides an opportunity to identify diabetes earlier in the process, before extensive damage occurs.
If a blood test reveals high fasting insulin before glucose and Alc become elevated, this provides an opportunity to identify diabetes earlier in the process, before extensive damage occurs.
Published data suggest elevated fasting insulin can be a useful diagnostic tool for identifying early-stage insulin resistance.24
One study found insulin resistance to be the most important predictive risk factor in the development of coronary artery disease.25
Other studies recognize the prognostic value of fasting insulin and suggest that hyperinsulinemia (high fasting insulin) is often both a result and a driver of insulin resistance.16
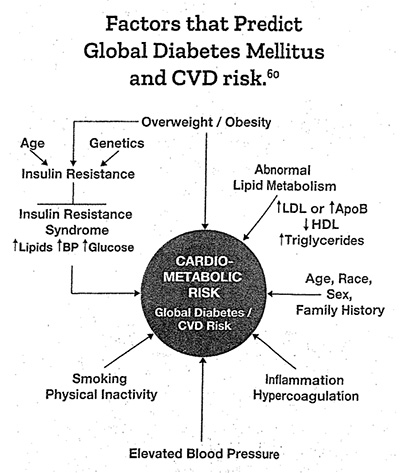
A consistent association exists between hyper¬tension (high blood pressure) and elevated insulin.26
Mechanistic factors have been identified to explain why tissue damage associated with “excess” insulin and insulin resistance causes blood pressure to spike.27
Kidney Damage
Chronic kidney disease is surging, coinciding with an increased prevalence of obesity, hypertension, and diabetes.
Insulin resistance and hypertension predispose to premature atherosclerosis28,29 and other pathologies that contribute to chronic kidney disease.21,32
Cardiometabolic syndrome, (a constellation of metabolic dysfunction characterized by insulin resistance, impaired glucose tolerance, dyslipidemia, hypertension, and intra-abdominal obesity) is associated with an increase in cardiovascular disease33,34 and kidney failure.35,36
Recognition of the role of insulin resistance and hyperinsulinemia in cardiometabolic syndrome provides a rationale to measure fasting insulin blood levels.
Based on the currently available data, we believe that fasting insulin above 5 pJU/mL is likely suboptimal. Steps that can be taken to improve metabolic health include a healthy, plant-based diet low in simple sugar, processed animal products, and saturated fat, and high in nutrients that help support metabolic health.37
Physical activity is also important for metabolic health.
Along with these lifestyle changes, and if appropriate for an individual based upon his/ her unique health needs, the use of medications under a physician’s care, including mefformin38,39 and/or an SGLT2 inhibitor40.41 like Jardiance® can further improve metabolic health before full-blown type II diabetes manifests.
Advanced-stage kidney disease is currently irrevers¬ible. Identifying causative risk factors early with blood tests that include fasting insulin can enable one to take corrective actions in time.
Cancer
 Insulin has direct and indirect effects on cancer cell progression, proliferation, and metastasis.42,43
Insulin has direct and indirect effects on cancer cell progression, proliferation, and metastasis.42,43
Studies investigating the association between hyperinsulinemia and cancer-related mortality have been inconsistent. Reasons might include the upper-limit reference range used to define hyperinsulinemia.
For example, the standard reference range for fasting insulin begins at 2,6 uIU/mL and extends to a startling high of 24.9 ulU/mL.”
Life Extension® long ago urged readers to target fasting insulin below 7.0 ulU/mL with optimal fasting insulin below 5.0 ulU/mL.
Today’s laboratory reference ranges don’t define hyperinsulinemia until fasting insulin rises above 24.9 ulU/mL. This is 3-to-5-times higher than what we consider optimal.
A study found lung cancer incidence doubled in men in the highest quartile of fasting insulin compared to those in the lowest insulin quartile. The conclusions from this study were:
“Higher fasting serum insulin concentrations,
as well as the presence of insulin
resistance, appear to be associated with
an elevated risk of lung cancer.”45
A gender-based subgroup analysis of seven different studies found significant association between fasting insulin and cancer mortality. The risk of cancer mortality in men with high insulin levels is almost double as compared to those having lower fasting insulin levels.42
Ignorance regarding “optimal” fasting insulin levels might be obscuring the impact of high, but “normal” insulin resistance markers on cancer risk and overall cancer mortality.
Why the controversy?
Life Extension° has published articles over the decades about the disease risks associated with excess fasting insulin.
Yet there are inconsistencies in the literature and in medical opinion as to what levels of fasting insulin increase disease risks.
One impediment in reaching consensus is varying definitions.
Hyperinsulinemia and Cancer
A massive review article (369 references) published in 2021 describes the health risks and mechanistic dangers of excess insulin.46
What follows is an excerpt from this review titled: “Hyperinsulinemia in Obesity, Inflam¬mation and Cancer”:
“Hyperinsulinemia was associated with a 2-fold risk of cancer death.47
This increase of cancer mortality is also observed in people with normal body weight if they had hyperinsulinemia.48
Therefore, hyperinsulinemia is associated with increased risk of both cancer incidence and death. However, unlike hyperglycemia, there is no widely accepted insulin concentration to define hyperinsulinemia, so it is difficult to compare across studies. Nevertheless, the rationale to study the contribution of hyperinsulinemia to cancer is strong.”
Hyperinsulinemia is sometimes defined as:46
“The amount of insulin in blood being
higher than considered normal.”
With laboratory reference ranges defining “normal” as high as 24.9 ulU/mL, doctors who test fasting insulin may not realize the risks in patients with higher than optimal insulin levels.
We believe fasting insulin levels above 5.0-7.0 ulU/mL may indicate cellular insulin resistance, yet today’s laboratory reference ranges define normal as between 2.6 and 24.9 ulLi/mL.
A better definition of hyperinsulinemia is a condition in which:
“There are excess levels of insulin circulating
in the blood relative to glucose.”
Even this definition can make interpretation of blood test results challenging since the majority of Americans today are overweight and prone to large fluctuations in fasting glucose and insulin levels.
Even thin people can suffer from insulin resistance, which is another reason for testing blood for fasting insulin.
A mass education program about insulin resistance is urgently needed, along with knowledge that it can be detected early by properly interpreting fasting insulin, glucose and Alc blood test results.
What you can do today!
Insulin resistance can be reversed by aggressive dietary and lifestyle changes, including increases in physical activity.40,49-54
Nutrients with glucose-lowering effects can help in combination with diet and more physical activity. For some this is not enough, and for these individuals, medications like metformin and/or an SG LT2
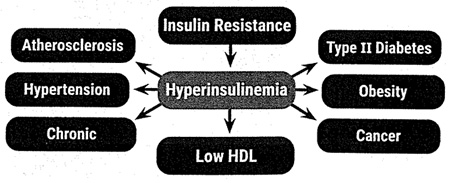
Hyperinsulinemia is a risk factor for other diseases.
Excess insulin and insulin resistance cause deleterious changes in many biochemical pathways that can lead to a number of degenerative diseases and potentially life-threatening metabolic consequences.
inhibitor may also be needed to optimize metabolic health. SGLT2 inhibitors are sold under brand names that include Jardiance®, Farxiga®, Invokana® and others.
An AMPK-activating drug called metformin improves insulin sensitivity and can reduce fasting insulin levels indirectly, largely as a result of improvement in peripheral insulin sensitivity at the cellular leve1.49,55
Sodium-Glucose Co-Transporter 2 inhibitor (SGLT2 inhibitor) drugs increase urinary excretion of glucose from blood. This drug class helps reduce the progression of chronic kidney disease in patients with type II diabetes and reduces adverse cardiovascular outcomes in many of these patients.56
Some studies show SGLT2 inhibitors reduce fasting insulin, likely a result of the reduction of excess blood glucose.57-69
The first step, however, is blood tests that measure glucose, Alc and fasting insulin.
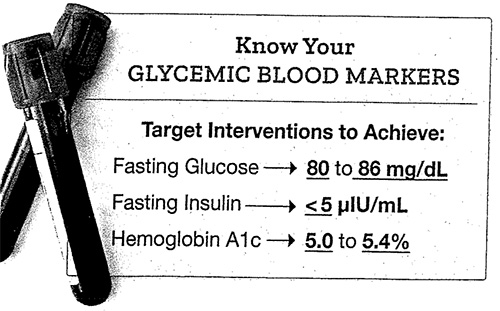
We suggest you target:
- Fasting Glucose between 80-86 mg/dL
- Hemoglobin A1c between 5.0%-5.4%
- Fasting Insulin <5 plU/mL
While these numbers are not achievable by everyone, you can at least lower them to safer ranges by initiating steps to improve glycemic status.
A popular blood test panel outlined on the next page includes Al c, glucose, fasting insulin, lipids, C-reactive protein, and other measures.
Commercial labs charge about $2,000 for these tests, but once a year we discount the popular Male and Female Panels down to $224.
You can order these tests 24 hours/day by calling 1-800-208-3444 or visting www.LifeExtenson.com/bloodtests
I hope this editorial explains why fasting insulin is included in many of our comprehensive blood test panels.
The article on page 24 of this issue describes an easy-to-take fiber approved by the FDA in 2020. One of the benefits found with this soluble plant fiber is reduced glucose and insulin blood levels.
For longer life,
Cellular Insulin Resistance
 The cells of many people with impaired glycemic control tend to be more resistant to insulin-stimulated glucose uptake than those with normal glucose tolerance.
The cells of many people with impaired glycemic control tend to be more resistant to insulin-stimulated glucose uptake than those with normal glucose tolerance.
The ability of insulin to stimulate cellular glucose uptake varies widely among individuals.
Resistance to insulin-stimulated glucose uptake and compensatory hyperinsulinemia represents a basic defect in many patients in the early stage of type II diabetes.1
As the condition worsens, insulin-producing pancreatic cells fail, thus some type II diabetics to require insulin injections.1
Increases in pancreatic insulin production can temporarily prevent elevations of glucose and Alc. This does not mean that this compensatory (hyperinsulinemic) response is benign.
Early-stage diabetic development (and related complications) is predictable by including fasting insulin with conventional blood test panels.

Leave a Reply